The only approved way to get vaccinated against COVID-19 is through a good ‘ol shot in the arm.
Eventually, West Virginia University medical researchers could change that narrative.
Scientists say they’ve developed a nasal mist that you would inhale through your nose and would offer protection against SARS-CoV-2 and its emerging variants.
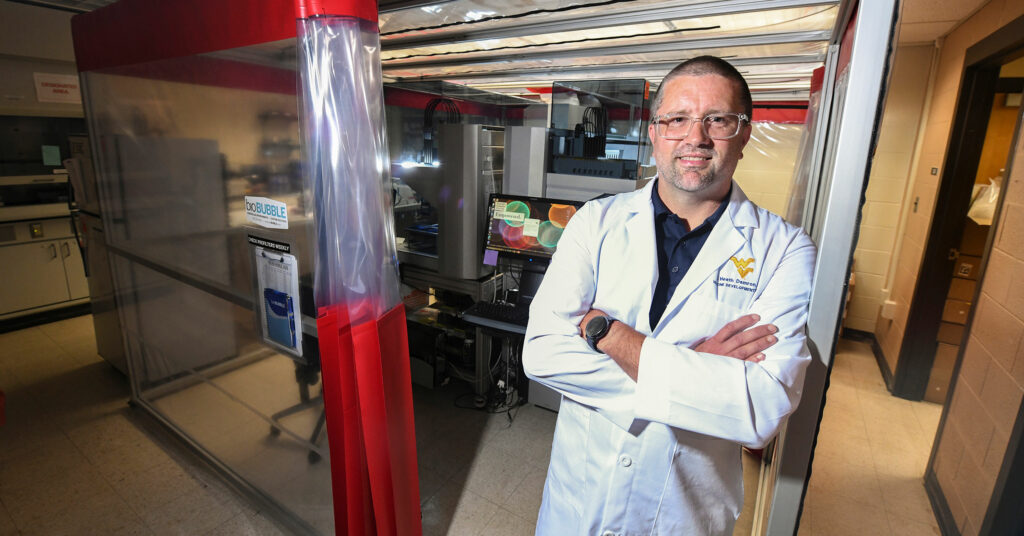
“The more I watched the vaccine race as a bystander, I kept thinking, ‘We should really test the idea of a nasal mist,’” said Heath Damron, director of the WVU Vaccine Development Center.
After all, the flu vaccine is offered nasally – and the fear of needles has led to some COVID-19 vaccine hesitancy, he continued.
For years, the Vaccine Development Center has worked on nasal vaccines for pertussis, widely known as whooping cough. Applying that knowledge to the COVID pandemic seemed like the natural thing to do.
In studying pertussis, researchers found that administering vaccines nasally instilled strong IgG antibody responses. IgG is the most common type of antibody in the blood and body fluids that “remembers” what it’s been exposed to before.
When COVID-19 dominated the globe in early-2020, Damron and his colleagues developed assays and their own antibodies for use in laboratories. They even tested out proteins they’d produced as vaccine components.
“At first, we tested by nasal and muscular vaccinations but didn’t get incredible antibody responses,” Damron said. “It was nothing you wanted to patent.”
Researchers then took the protein produced in-house and fused it with a carrier protein for a larger, high-molecular weight protein. Still no jackpot.
So they added to the mix an adjuvant, which is an immune stimulator, and as Damron explained, it “generated really elegant antibody responses.”
In essence, they produced an experimental vaccine composed of a bacterial cell wall component mixed with a SARS-CoV-2 antigen.
“It’s very interesting because we’re using something that looks like bacteria to cause airway inflammation to protect against a viral pathogen,” he said. “It’s simulating a light infection of bacteria to prepare for a viral invasion. Sometimes infections of one disease can protect against another.”
For the studies, Damron’s team developed models that express the ACE2 receptor, a protein on the surface of certain human cells. The SARS-CoV-2 virus, which has been widely depicted as a spikey ball, binds their spikes to the ACE2 receptor similarly to how a key fits into a lock.
When researchers nasally vaccinated animal models, 90 percent lived whereas those unvaccinated died at an 80 percent rate.
Researchers even observed the nasal vaccine to be more effective than if administered into the muscles, Damron said. He explained that a high amount of IgA antibody gets released into the nose and lungs, forging a wall of protection at the site where viruses begin to replicate.
“It (the IgA) will stick to the virus and keep it from getting into the cell,” Damron said. “It’s like a numbers game, if you can get enough to slow it down at the early stages of infection. There may still be some disease, but you don’t become massively infected.”
Damron’s team also observed that IgG antibodies increased as the infection persisted.
“When we provided our vaccine on the animal test models, and then administered the COVID-19 virus, they were running around like nothing ever happened,” said Damron, who’s also associate professor in the WVU Department of Microbiology, Immunology and Cell Biology.
Damron and his colleagues are continuing to evaluate the nasal mist vaccine against currently circulating strains including the delta variant. The team is looking for commercial partners to help facilitate production at scale and further clinical evaluation.
“We’re going to continue to investigate nasal and even oral vaccination strategies, not just from a COVID perspective, but also from a general vaccine perspective,” he said. “That’s why the research is important to happen in the academic setting because with most established vaccines, manufacturers are focused on the existing technologies they’re already good at. Nasal and oral strategies need more research behind them that can happen at top research universities like ours.”
From WVU Today