 When communities face epidemics of drug abuse, a wave of infectious diseases often follows, including hepatitis and HIV. A new federally-funded program in southern West Virginia, led by West Virginia University, will seek to interrupt that cycle.
When communities face epidemics of drug abuse, a wave of infectious diseases often follows, including hepatitis and HIV. A new federally-funded program in southern West Virginia, led by West Virginia University, will seek to interrupt that cycle.
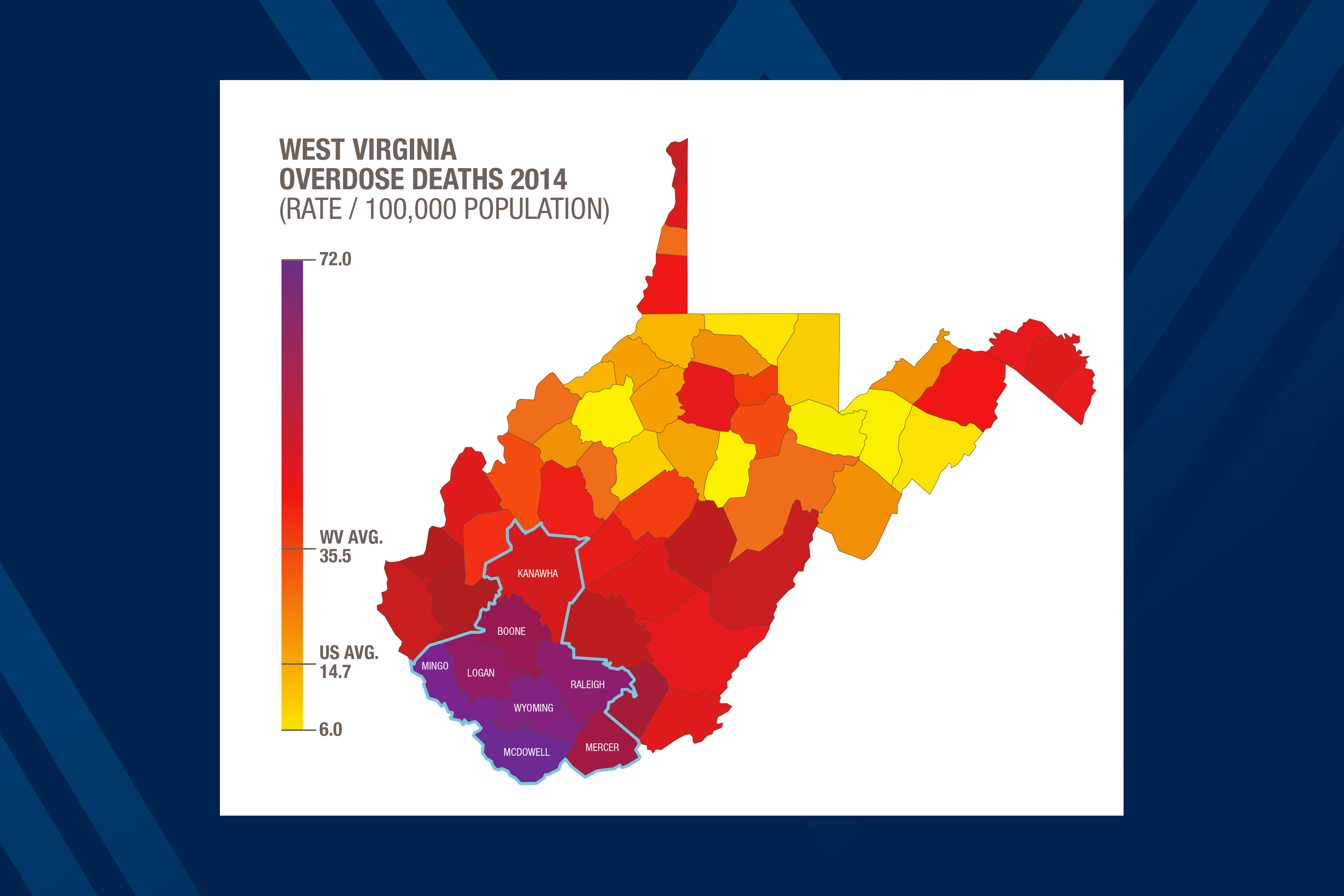
“West Virginia has the highest drug overdose fatality and hepatitis rates in the U.S.,” said Judith Feinberg, M.D., of the WVU School of Medicine. “We have not seen an HIV outbreak yet. But it’s a ticking time bomb for us, especially in rural areas where the local health system’s ability to detect and mitigate an HIV outbreak may not be well developed.”
The program, which combines research, health services, and community involvement in harm reduction strategies, will target eight West Virginia counties: Boone, Kanawha, Logan, McDowell, Mercer, Mingo, Raleigh and Wyoming. Six of the eight are among the top 25 counties in the U.S. in their per capita overdose fatality rates, according to the U.S. Centers for Disease Control and West Virginia statistics.
“The threat of an HIV outbreak here is among the highest in the U.S.,” said Gordon Smith, M.D., MPH, Stuart M. and Joyce N. Robbins Distinguished Professor at the WVU School of Public Health. “Based on the CDC’s analysis of a 2014-15 outbreak of HIV and hepatitis C in rural Indiana, and the high rates of poverty, overdose deaths, and hepatitis B and C infections we see in this region, it would not take long for a small number of HIV cases to set off a serious health crisis.”
Feinberg and Smith are co-leaders of a project that will develop an integrated prevention, harm reduction and treatment team across the region in partnership with local communities to rapidly identify and mitigate small HIV “microepidemics,” and keep them from spreading to a larger number of people.
“The success of this approach will be driven by input from local communities and public health agencies,” Feinberg said. “We will work with them to coordinate and improve screening, prevention and treatment for hepatitis C, HIV and other infections associated with injection drug use.”
The first phase is a two-year effort to develop an evidence-based road map, working with local communities and public health agencies, to coordinate and improve screening, prevention and treatment for hepatitis C, HIV and other associated diseases,” Smith said. “It also involves developing a novel strategy to rapidly identify the emergence of HIV and other complications of injection drug use in isolated rural communities and use it to target communities at highest risk. If this first planning phase is successful, increased funding for a further three years will enable “…implementation of a comprehensive program to prevent the devastating effects of injection drug use in these hard-hit communities.”
The project is titled Rural West Virginia Responds to Opioid Injection Epidemics: From Data to Action and is supported by a $1,010,068 grant for two years from the National Institute of Drug Abuse, a part of the National Institutes of Health, the Centers for Disease Control and Prevention, and the Appalachian Regional Commission. It is also supported by the Substance Abuse and Mental Health Services Administration and the West Virginia Clinical and Translational Science Institute.